 Turning a patient’s own immune system against their cancer has long been considered the Holy Grail of cancer therapy.
Turning a patient’s own immune system against their cancer has long been considered the Holy Grail of cancer therapy.
For hundreds of years scientists, physicians, herbalists, and many, many non-scientists have endeavored to accomplish this. Despite billions of dollars spent and many false claims made, only recently has this come to fruition.
Two new medicines are leading this revolution in cancer treatment, and they work a little differently than you might think.
These new immune treatments don’t just “boost” or “activate” the immune system (as many Internet-based, non-approved immune therapies claim to do). It’s not so simple.
Our immune systems are highly complex, involving dozens of cells and chemicals that work in concert to first recognize the target (such as an infectious agent) and then attack and eliminate it. Once the target has been eliminated, the immune attack must stop or it would cause injury to the body.
Think of an infection you may have had, on your skin or internally, such as a urinary tract or respiratory infection. You experience the symptoms of the infection, such as fever, malaise, burning urine or cough, and then as your immune system battles the infection successfully (often with the aid of antibiotics), you feel the healing of recovery. The attack is over and your immune system quiets down.
It is this process of “putting the brakes on” that the new immune therapies harness.
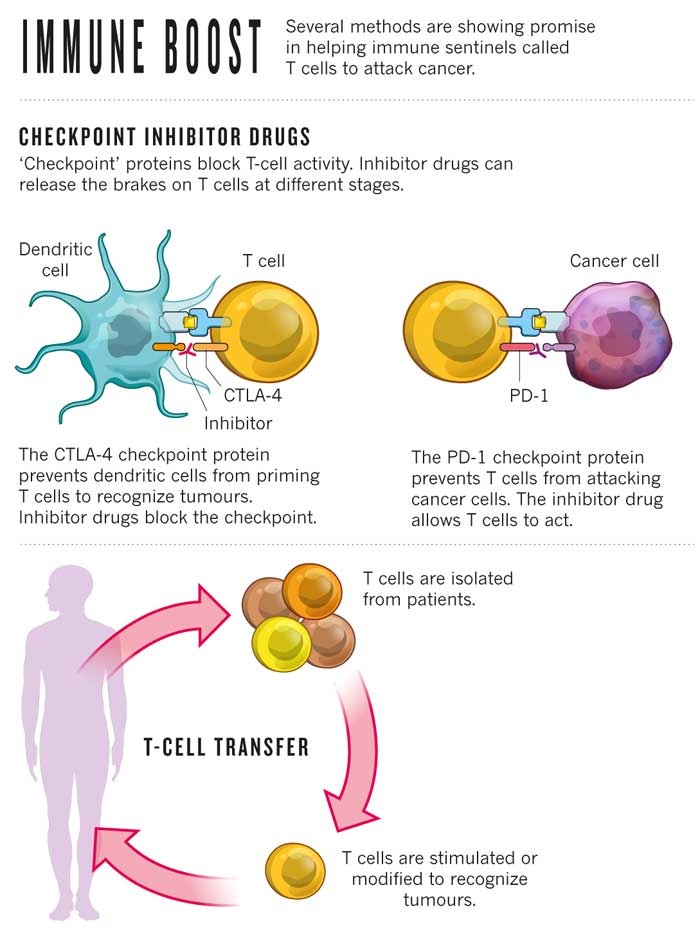
The therapies target proteins on our immune cells: PD-1 and CTLA-4. Both PD-1 and CTLA-4 exist as antennae or receptors on the surfaces of immune cells to stop the immune attack once it has done its job.
It turns out that cancer cells also employ PD-1 and CTLA-4 to prevent immune cells from recognizing them. The new medicines ‘block the blockers’ and release the brakes on the immune system’s attack on cancer cells.
In 2011, ipilimumab (Yervoy), which blocks CTLA-4, was approved by the US Food and Drug Administration to treat metastatic melanoma. Recently, pembrolizumab (Keytruda), which blocks PD-1, was also approved to treat melanoma. But the activity of these medicines goes far beyond melanoma. A publication in the New England Journal of Medicine in 2012 first showed that blocking PD-1 can result in cancer remissions in the most difficult cases of lung and kidney cancers. Other types of cancer, such as those derived from the bladder and ureter appear particularly susceptible to PD-1 targeting drugs. There is now an explosion of medicines in this class and of clinical trials testing their activities against nearly every type of incurable cancer. Plus, drugs like Yervoy and Keytruda are being combined in some trials, perhaps to greater effect than when either drug is used alone.
Although these drugs can have side effects (as all anti-cancer drugs do), the beauty of this kind of treatment is that the immune system “remembers what it targets” so that the control of the cancer within may be very long lasting.
As Dr. Antoni Ribas wrote in an editorial in the New England Journal of Medicine, “The use of PD-1 blockade may well have a major effect on cancer treatment.”
WebMD: October, 2014. By Richard C. Frank, MD
Go to www.clinicaltrials.gov to find clinical trials testing these new immune therapies.